BLOG • Feb 19, 2025
Unlocking Revenue Potential: Why CARC Codes Are Essential for Denial Management
Dedicated to Delivering High-Quality Risk Adjustment Coding
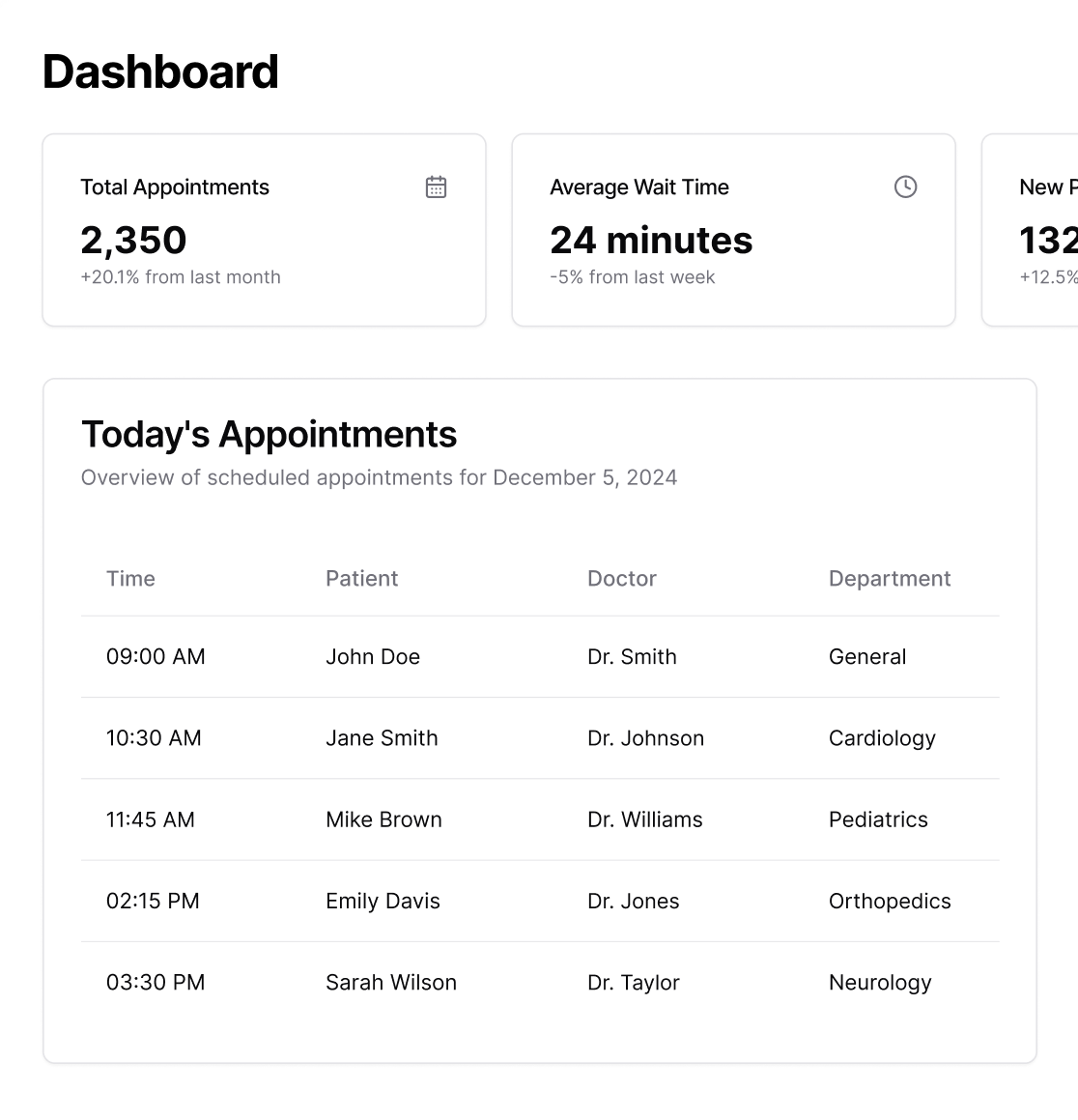
Schedule a CallTotal Appointments Scheduled
No-Show Rate
Providers Available
From prospective and concurrent reviews to targeted chart evaluations and advanced validation processes, each method plays a crucial role in improving coding accuracy and aligning with regulatory requirements
Our certified coding specialists focus on HCC coding, precisely recording patient conditions to represent their actual health status and risk ratings.
We thoroughly evaluate patient charts and data to identify missing or inaccurate diagnoses.
We employ cutting-edge workflow management technologies to expedite turnaround times, increase efficiency, and simplify coding
We employ cutting-edge workflow management technologies to expedite turnaround times, increase efficiency, and simplify coding
We provide in-depth data and analytics to help you comprehensively understand your risk adjustment performance
ASP-RCM coders deliver accurate, compliant risk adjustment coding that meets client expectations. We follow current CMS and HHS guidelines, use strict quality checks, and ensure all codes are backed by proper documentation. Our process helps clients improve RAF scores, reduce audit risk, and get reliable financial projections. We focus on complete, correct coding—nothing missed, nothing unsupported.
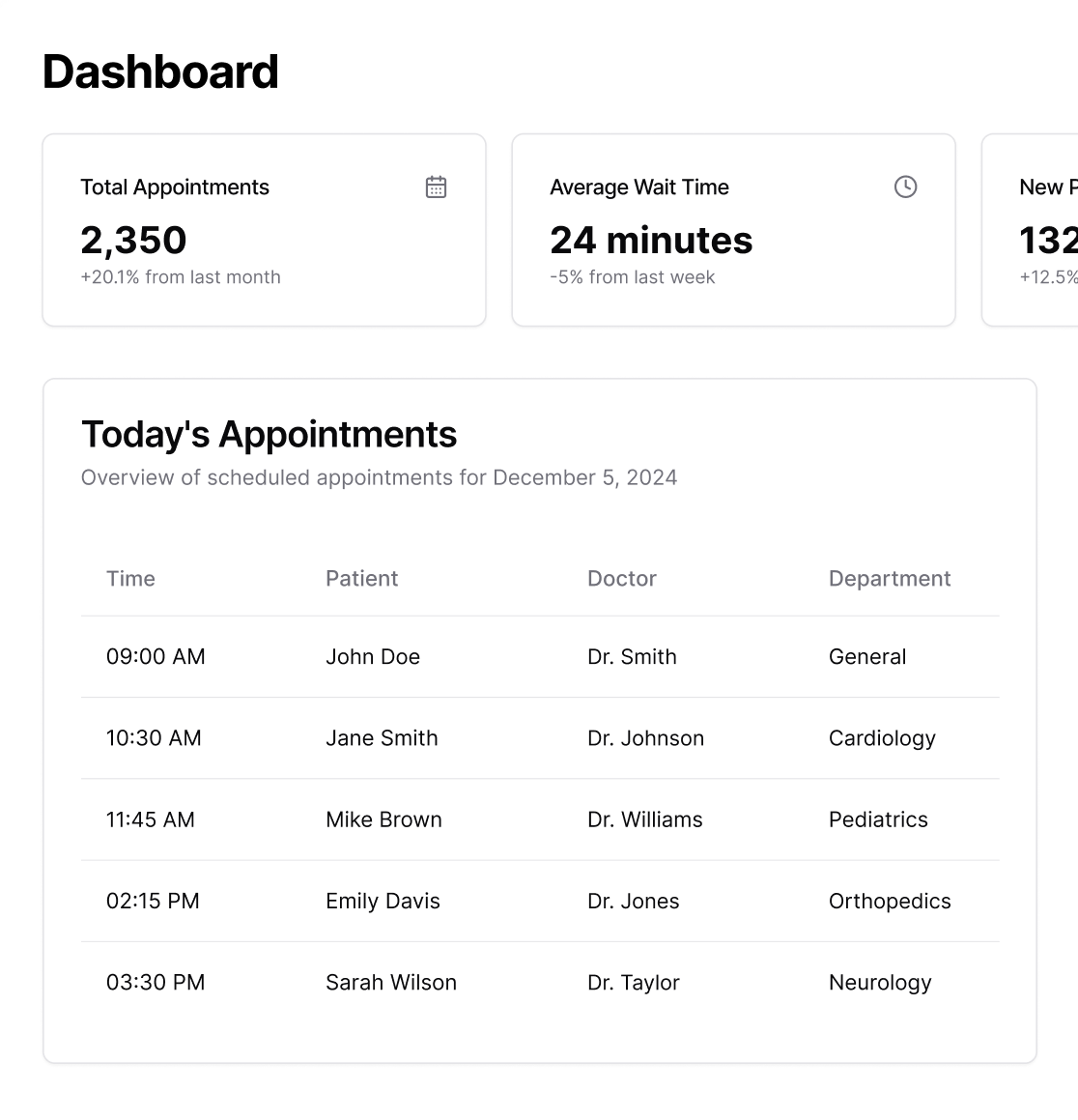
At ASP-RCM, our coders conduct prospective reviews before patient visits to flag potential risk adjustment opportunities. We review historical data, identify missing chronic conditions, and highlight suspect diagnoses that require provider validation. What sets us apart is our ability to combine coding expertise with clinical insight, ensuring providers are prepared to document conditions accurately during the encounter. This proactive approach helps close gaps, improve capture rates, and support stronger RAF scores.
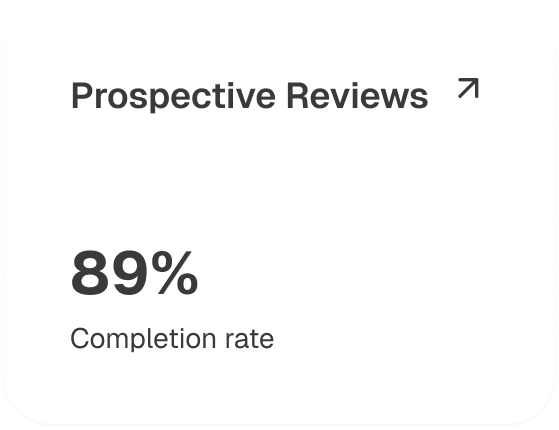
While care is underway, we monitor documentation in real time to keep coding aligned with the evolving clinical picture. ASP-RCM works side by side with care teams to validate diagnoses, capture emerging conditions, and meet payer requirements before discharge. This live oversight keeps revenue secure, reduces denials, and ensures claims are accurate the first time.
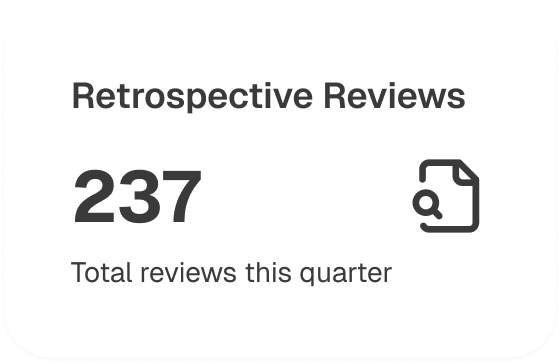
After the encounter, our team conducts a thorough review to catch what others overlook. ASP-RCM analyzes records for missed diagnoses, incomplete documentation, and risk adjustment opportunities—well before claims or audits create exposure. The result: corrected records, maximized reimbursement, and a complete clinical story backed by compliance confidence.
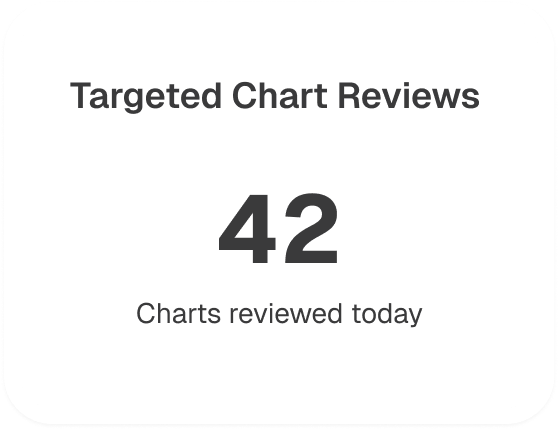
When a specific diagnosis, condition, or service is in question, ASP-RCM zeroes in. Our targeted chart reviews focus on high-impact areas—like chronic conditions, complex procedures, or documentation flagged for payer scrutiny. By addressing only what matters, we deliver fast, accurate insight that strengthens claims and reduces the risk of denials.
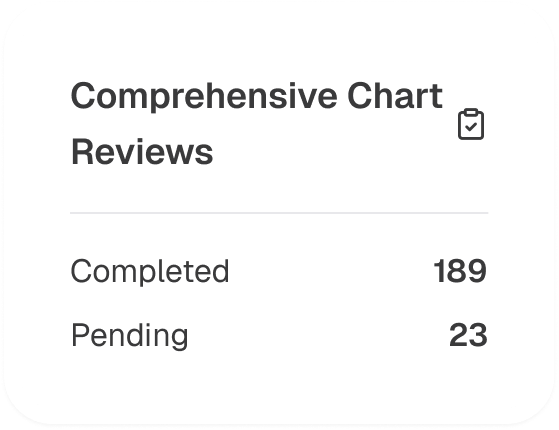
We check everything to get a whole picture. The thorough reviews conducted by ASP-RCM examine every patient record, noting all diagnoses, verifying paperwork, and guaranteeing correct coding for each encounter. A fully optimized chart that promotes clinical integrity, audit preparedness, and proper reimbursement is the end result.
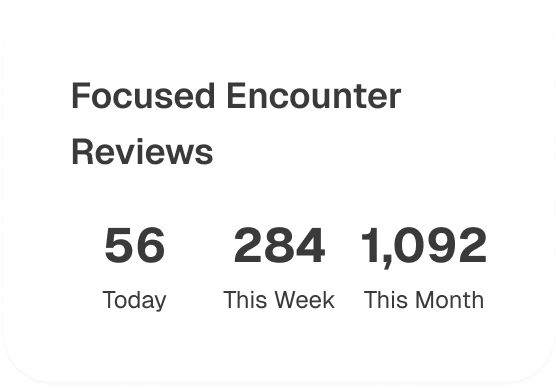
High-stakes encounters demand precision. ASP-RCM zeroes in on visits like Annual Wellness and hospital admissions, validating documentation, confirming coding accuracy, and addressing gaps before claims go out the door. The result: protected revenue, fewer denials, and compliance locked in from the start.
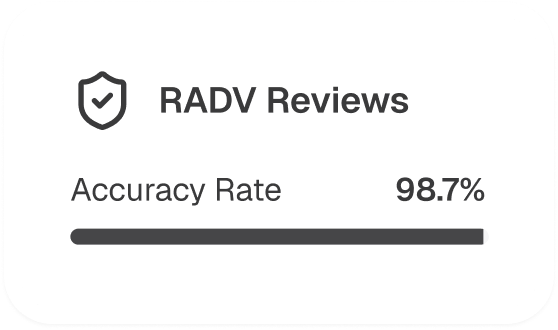
RADV reviews leave no room for error. ASP-RCM applies the same scrutiny payers use—verifying every coded diagnosis against the medical record. We pinpoint weak spots, correct inconsistencies, and equip providers to defend their risk adjustment data with full confidence.
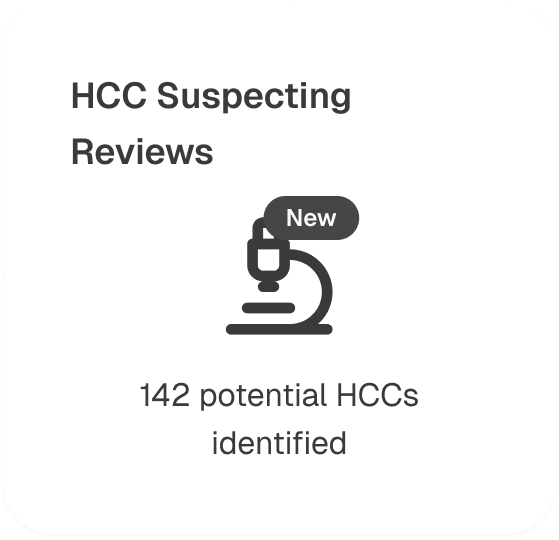
Identifying potential risk conditions before they impact scores is where ASP-RCM excels. Our HCC suspecting reviews leverage patient history and clinical patterns to flag likely chronic conditions that may be under-documented. This ensures providers have the insight needed to confirm, document, and capture risk accurately.
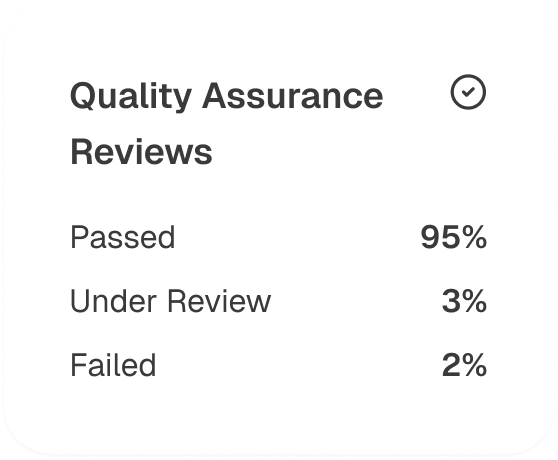
Strong claims start with airtight processes. ASP-RCM’s quality assurance reviews audit coding accuracy, verify documentation, and ensure compliance with CMS and industry standards. This final checkpoint protects revenue, prevents costly rework, and keeps your organization audit-ready year-round.
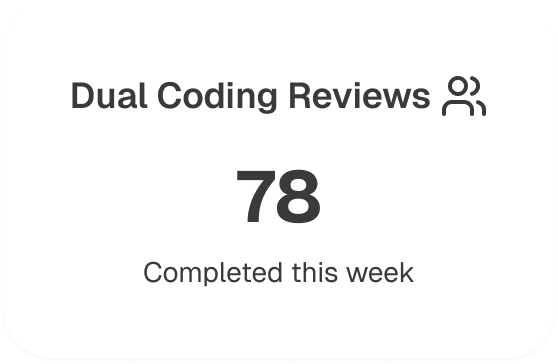
For critical encounters, ASP-RCM assigns two independent coding teams to review the same record. Every code is verified for accuracy, every discrepancy resolved. This extra layer of scrutiny elevates coding precision, reinforces compliance, and strengthens payer confidence.
Share your details with us, and we'll set up a tailored demo just for you.
